(News from Nanowerk) Daegu Gyeongbuk Institute of Science & Technology (DGIST, President Yang Kook) Professor Hongsoo Choi’s team from the Department of Robotics and Mechatronic Engineering collaborated with Professor Sung-Won Kim’s team at St. Mary’s Hospital in Seoul, Catholic University of Korea, and Prof. Bradley J. Nelson’s team at ETH Zurich to develop technology that produces over 100 microrobots per minute that can be disintegrated in the body (Little“A biodegradable magnetic microrobot based on gelatin methacrylate for precise stem cell delivery with mass production capability”).
Microrobots aimed at minimally invasive targeted precision therapy can be fabricated in different ways. Among them, the ultra-fine 3D printing technology called two-photon polymerization method, a method that triggers polymerization by crossing two lasers in synthetic resin, is the most widely used. This technology can produce a structure with nanometric precision.
However, a disadvantage exists in that the production of a microrobot takes time because the voxels, the pixels made by 3D printing, must be cured successively. In addition, the magnetic nanoparticles contained in the robot can block the path of light during the two-photon polymerization process. This process result may not be uniform when using high concentration magnetic nanoparticles.
To overcome the limitations of the existing microrobots manufacturing method, DGIST Professor Hongsoo Choi’s research team developed a method to create microrobots at a high speed of 100 per minute by flowing a mixture of magnetic nanoparticles and methacrylate of gelatin, which is biodegradable and can be cured by light, into the microfluidic chip. That’s over 10,000 times faster than using the existing two-photon polymerization method to make microrobots.
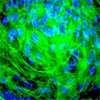
Then, the microrobot produced with this technology was cultured with human nasal stem cells taken from the human nose to induce the adhesion of stem cells to the surface of the microrobot. Through this process, a microrobot carrying stem cells, comprising magnetic nanoparticles inside and stem cells attached to the outer surface, was made. The robot moves when the magnetic nanoparticles inside the robot react to an external magnetic field and can be moved to a desired position.
Selective cell delivery was difficult with existing stem cell therapy. However, the stem cell-bearing microrobot can move to a desired location by controlling the magnetic field generated by the real-time electromagnetic field control system.
The research team conducted an experiment to examine whether the stem cell-carrying microrobot could reach the target point by passing through a maze-like microchannel, and therefore confirmed that the robot could move to the desired location.
Additionally, the degradability of the microrobot was assessed by incubating the stem cell carrying the microrobot with a degrading enzyme. After 6 h of incubation, the microrobot was completely disintegrated, and the magnetic nanoparticles inside the robot were collected by the magnetic field generated by the magnetic field control system. Stem cells proliferated where the microrobot was disintegrated. Subsequently, the stem cells were made to differentiate into nerve cells to confirm normal differentiation; the stem cells differentiated into nerve cells after about 21 days.
This experiment verified that the delivery of stem cells to a desired location using a microrobot was possible and that the delivered stem cells could serve as a precision-targeted therapeutic agent by exhibiting proliferation and differentiation.
Additionally, the research team confirmed whether the stem cells delivered by the microrobot showed normal electrical and physiological characteristics. The ultimate goal of this study is to ensure that the stem cells delivered by the robot normally fulfill their role as a bridge in a state where the connection between existing nerve cells is disconnected.
To confirm this, hippocampal neurons extracted from rat embryos that stably emit electrical signals were used. The corresponding cell was attached to the surface of the microrobot, cultured on an electrode microchip, and electrical signals were observed from hippocampal neurons after 28 days. Thanks to this, the microrobot has been verified to correctly fulfill its role as a cell delivery platform.
Professor Hongsoo Choi of DGIST said: “We expect that the technologies developed in this study, such as mass production of microrobots, precise operation by electromagnetic fields and delivery and differentiation of stem cells , greatly increase the effectiveness of targeted precision therapy in the future. ”





More Stories
Delay in mass production of new Intel products is a boon for AMD, share of AMD x86 server processors expected to exceed 22% in 2023, according to TrendForce
Quantum industry milestone brings mass production of quantum chips closer
NEO Battery Materials provides updates on installation of additional equipment for mass production optimization and final stages of commercial plant design for construction